DEFINE: A lung disease that is a combination of chronic bronchitis and emphysema. This disease limits airflow due to inflammation and C02 retention. These individuals often have a chronic cough, wheezing, shortness of air, and increased mucus production. The also generally have destruction of inter-alveolar septa destruction. Alveoli sacs are where 02 and C02 exchange happens.
RISK FACTORS:
1. Smoker
2. Alpha 1 antitrypsin deficiency
3. Chemical irritant exposure
SUBJECTIVE:
1. Shortness of air
2. Wheezing
3. Tight chest
4. Increased mucus production
PHYSICAL EXAM: (HALLMARK SIGNS=**)
1. Barrel chest
2. Clubbing fingernails
3. Wheezes**
4. Rhonchi
5. Decreased lung sounds
6. Thick sputum**
7. Percussion: hyper-resonance
8. Cyanosis
LABS:
1. Spirometry; FEV1/FVC ratio <70%
2. CBC- may see elevated hit
3. Pulse oximetry: Varies from patient to patient but often seen 88-92%
4. ABG: C02 is often elevated
5. D-dimer
6. Continuous pulse oximetry
7. A1-antitrypsin screen (specifically in those <45 yrs old)
8. CXR: Hyperinflation
9. PFT
10. Sleep studies
11. Sputum culture
STAGES: (FEV1=Amount of air that can be forcefully expelled in 1 second)
1. Stage 1- Mild FEV1 80% greater than or equal to this. May have some mild shortness of air and increase mucus. Also an ongoing chronic cough
2. Stage 2- Moderate FEV1 between 50-79%
3. Stage 3-Severe FEV! Between 30-49%
4. Stage 4- END STAGE Very severe. FEV1 <30%
5. Lung transplant. 02 around the clock
MEDICATIONS COMMONLY USED:
1. Short acting B-agonist: Example: Albuterol scheduled and PRN
2. Anticholinergic-example: Ipratropium, Tiotropium. These meds ease the airways
3. Long Acting B-agonist: Salmeterol, Formoterol
4. Expectorants
5. Oxygen (typical 2-3 L in pm)
ACUTE CARE:
1. IV steroids
2. Empiric antibiotic
3. 02 nasal cannula
RISK FOR ACUTE FLARES:
1. Recent URI
2. Influenza
3. Allergies
4. Environmental irritants
5. Weather changes
TEACHING
1. Vaccination- pneumovax & influenza recommended
2. Smoking cessation
3. Your airflow (in & out) is limited due to obstruction, thus you may have ongoing mild shortness of air. If you shortness of air suddenly increases you should be seen ASAP by a medical healthcare
provider (Emergency Room)
4. Pursed lip breathing
5. Avoid triggers: cold air, infections, air pollutants, cigarette smoke
6. Eat smaller more frequent meals
REFERRALS
1. Pulmonologist
COMPLICATIONS:
1. Chronic anemia
2. Respiratory failure
3. Right ventricular hypertrophy
4. Recurrent lung infections
5. Cor pulmonale: right sided heart failure secondary to COPD
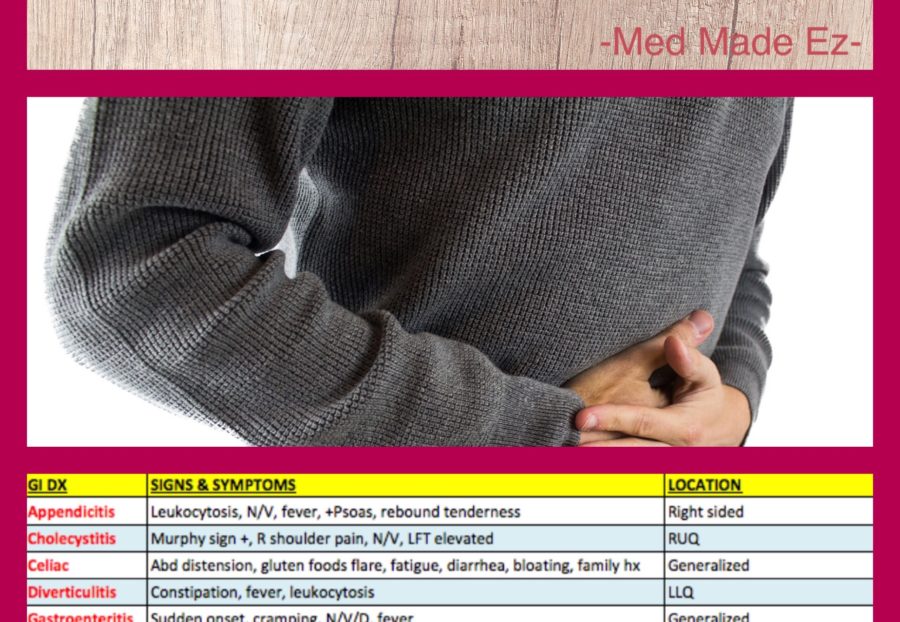
DIFFERENTIAL DIAGNOSIS (Dx that can appear similar)
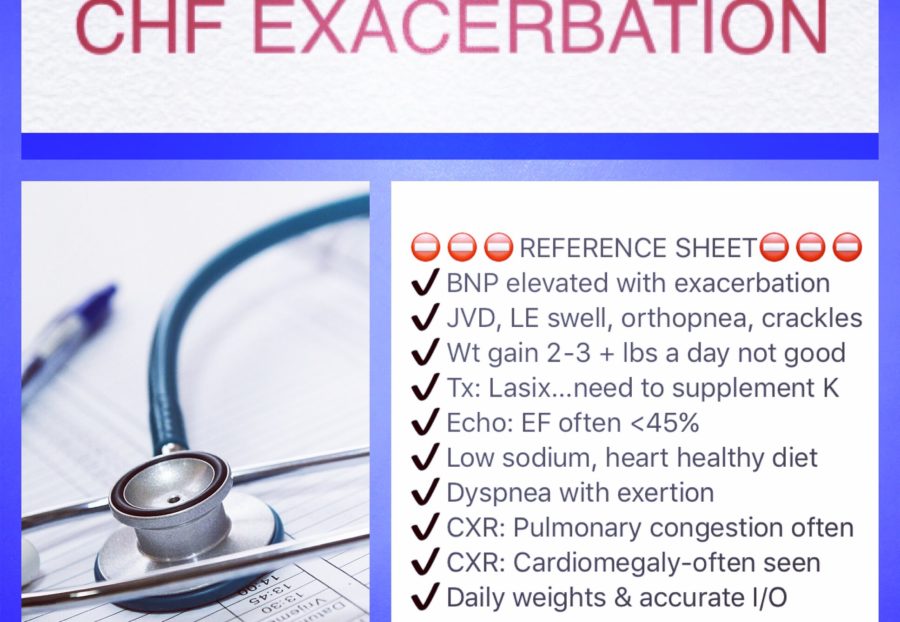
1. Congestive heart failure
2. Bronchitis
3. Pneumonia: Fever, more acute
4. Asthma: may be younger.
5. Lung cancer
6. Chronic pulmonary embolism
7. Bronchiectasis
8. Reactive airway
9. Bronchospasms
WORDS LINKED-ASSOCIATED
1. Emphysema
2. Blue Bloater
3. Pink Puffer
4. Hypoxic drive theory
5. Hypoxia
6. Hypercapnia
7. Spiromerty
8. FEV1
ONLINE RESOURCES:
1. American Lung Association http://www.lung.org/lung-health-and-diseases/lung-disease-lookup/copd/
2. National Heart, Lung, And Blood Institute http://www.nhlbi.nih.gov/health/health-topics/topics/copd
3. Medscape http://emedicine.medscape.com/article/297664-overview
4. COPD Foundation http://journal.copdfoundation.org
REFERENCES:
1. The 5-minute Clinical consult 2015 43rd Edition page 240. Alan J Crop MD, Bryon Veynovich. Editor in Chief Frank J Domino
2. Epocrates COPD May 2016
3. COPD Foundation http://www.copdfoundation.org/What-is-COPD/COPD-Facts/Glossary.aspx
4. Healthline, End-Stage COPD, Written by Rachel Nall, RN, BSN, CCRN Medically Reviewed by Mark R Laflamme, MD on November 19, 2015 http://www.healthline.com/health/copd/end-stage-copd#Overview1
5. UPMC Life Change Medicine http://www.upmc.com/patients-visitors/education/breathing/pages/chronic-obstructive-pulmonary.aspx
Update on May 2nd,2016